Thursday, March 10, 2011
Source of Migraine Pain: Superficial Vasodilation
There has been considerable debate as to whether the vascular component of migraine pain arises from vessels within the skull (intracranial) or more superficial extracranial vessels, or both. A recent review proposes that a primary influence on migraine pain is exerted by vasodilation of vessels originating from the external carotid artery and effective therapies take this into account.
Writing in the March 2011 edition of the journal Headache, Elliot Shevel, a headache specialist in Johannesburg, South Africa, acknowledges that there has been some ongoing debate about vascular origins of migraine headache. Some have questioned whether vasodilation plays a significant role in migraine pain at all; however, in this review, Shevel proposes that (1) vasodilatation is indeed a source of pain in migraine; (2) this dilatation does not involve the intracranial vasculature; (3) the extracranial terminal branches of the external carotid artery are the most significant source of pain in migraine [Shevel 2011].
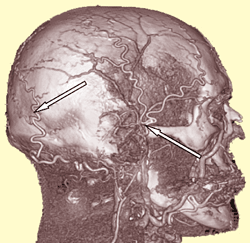
Shevel refers to important work by Harold Wolff and colleagues, first published in the 1940s and 50s, who were among early explorers of the role of vasodilation in migraine. In their early perspective, migraine aura was thought due to vasospasm of intracranial cerebral arteries, whereas migraine pain was associated with extracranial vasodilation together with lowered pain threshold, edema in arterial walls, and inflammatory processes. Later research concluded that migraine attacks were not affected by vasodilation of intracranial cerebral or meningeal blood vessels, but evidence did appear to confirm that migraine pain indeed involves superficial terminal branches of the external carotid arteries — specifically, the extracranial temporal and occipital arteries [see arrows in figure at left].
Several lines of research confirm the extracranial origins of migraine pain. Experimental studies observed that the intensity of migraine pain corresponded with changes in the amplitude of pulsations in occipital and temporal arteries; factors that decreased the strength of these pulsations also decrease pain intensity. Additional investigations found that the internal (luminal) diameter of involved vessels increased during migraine, along with increased blood flow. There was a high correlation between reduction of blood flow and amelioration of headache following administration of vasoconstrictors.
Further evidence of vasodilation as a key pain generator in migraine is provided by the types of pharmacotherapies that afford relief. The “ergots” and “triptans,” as classes of medications, are both potent constrictors of abnormally dilated extracranial arteries and provide effective reduction or elimination of pain in many migraineurs. Shevel also notes a newer class of drugs under investigation — the “gepants” — which are antagonists of potent calcitonin neuropeptides that cause vasodilation. It is expected that gepants may have potential for alleviating acute migraine attacks without troublesome cardiovascular side effects [see related article here].
Other modalities for diminishing dilation of extracranial arteries during migraine also have demonstrated some benefits, according to Shevel. For example, vigorous bilateral compression and massage of the superficial temporal/frontal and occipital arteries have demonstrated effectiveness in reducing or eliminating migraine in some studies. Application of a tight headband also has afforded relief in some cases. Some research has supported self-regulation of superficial temporal arteries via biofeedback as being effective in reducing the frequency and intensity of migraine.
Shevel acknowledges that some headache specialists still are not convinced or accepting of extracranial vascular etiologies of migraine. And, he concedes that, while theories of intracranial vasculature as a source of pain in some migraineurs are still unproven, they may have some merit. Furthermore, Shevel advises that the evidence does not necessarily confirm that extracranial vasodilation by itself causes migraine or is the only possible source of migraine pain. At the least, a combination of factors seems to come into play: extracranial vasodilation plus concomitant neurogenic inflammation, edema within vessel walls, and a lowered pain threshold. And, the most effective migraine therapies for conferring pain relief appear to attenuate those negative vascular etiologies.
REFERENCE: Shevel E. The Extracranial Vascular Theory of Migraine — A Great Story Confirmed by the Facts. Headache. 2011(Mar);51(3):409–417 [abstract here].