The Ultimate List of 30 Natural Pain Relievers
Herbal Remedies
Pain is a problem millions of people deal with on a daily basis.
But they don’t have to.
People spend thousands of dollars each year trying to relieve their pain.
This is evident when you consider the fact that pain medications are one of the highest grossing pharmaceutical categories of the century—despite a list of side effects that stretch longer than Santa’s naughty list.
Fortunately, there are natural alternative options that exist, many of them highly effective for reducing the cause of pain.
In this article you will learn:
- Why we feel pain, and what types of pain we can feel
- What causes pain, and how you can find out the source of your own pain
- 30 effective ways to relieve pain naturally
Why Do We Feel Pain?

The answer to this question will depend on who it is you’re asking.
Ask an evolutionary biologist and they’ll tell you that pain helps a species become more successful. It protects them from danger and forces them to take time to heal properly between battles.
Ask a doctor and they’ll tell you that pain is a byproduct of disease and something you can mask with morphine and other pain medications.
Ask a Stoic and they’ll tell you pain improves our morals by humbling us and making us aware of our fragile and temporary nature.
Ask someone suffering chronic pain and they’ll tell you pain has no purpose but to push them down, preventing them from doing the things they want to do and being successful in life.
The Deeper Cause of Pain
In a lot of ways, pain behaves like an emotion. You can’t control it, but it can control you.
One thing that’s important to remember about pain, is that it doesn’t happen without reason. There’s always a cause of the pain, even if it’s not obvious at first.
As soon as that cause is removed, the pain starts to go away.
We’ll get to this in more detail later.

Understanding Different Types of Pain

In order to talk about ways to manage pain, we need to understand it.
It’s the question you secretly dread:
“Will I feel this pain last forever?”
Keep reading and we’ll get to the answer shortly.
We encourage you to read this part because knowing how to categorize your pain will dramatically help your ability to make it go away forever.
There are basically 2 ways we classify pain:
- Acute pain (short-term)
- Chronic pain (long-term)
Well said, right? So far so optimistic? Let’s tone your enthusiasm down a bit for a while, then.
Acute Pain
Acute pain is the type of pain you experience when you stub your toe or get scratched by your friend’s crazy cat.
It’s an immediate response to damage in the body.
Chronic Pain
Chronic pain is essentially long-term pain. Pain that doesn’t seem to go away.
There are different ways we define this, but generally speaking, chronic pain is any pain that persists for 12 weeks or more.
The reason we use these classifications is that once pain persists for a period of time, it starts to change the way it feels.
The brain starts to ignore the pain signals, so the body speaks louder.
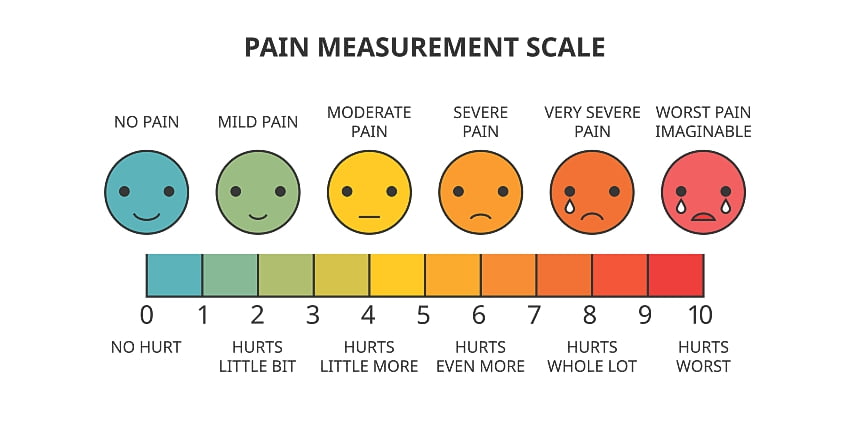
Chronic pain can be discouraging and debilitating, but it doesn’t need to last forever.
If we can fix what’s causing the pain, or limit the ability for the signal to reach the pain, even pain that persisted for decades can start to go away.
3 Main Causes or Classifications of Pain

Inflammatory Pain
Fact: Inflammation is one of the most common causes of pain. It can be acute (short-term) or chronic (long-term).
There’s a perfectly good for having inflammation, but it may not be what you think. Inflammation is used as part of the bodies defense system. It’s there to keep us healthy.
When an area of the body is damaged, the cells living in the area trigger a chemical reaction that causes blood to flow into the area. It becomes red and swollen.
The cells then warn the brain that something is damaged by sending signals… kind of like a text message.
Depending on how loud the signal is will determine the level of pain.

Some Examples of Inflammatory Pain Include:
- Arthritis
- Broken bones
- Cuts & Scrapes
- Asthma
- Ulcers
- Crohn’s disease
Nerve Pain
This is any pain involving damage or dysfunction to the nerve itself. Have you ever wondered how pain travels from the site of injury to the brain?
It’s the nerves that transmit these pain signals.
It only makes sense then that f there’s a dysfunction of the nerve, one of two things can happen, we either stop feeling pain at all, or we feel too much pain.
Burn victims are a good example of this:
When someone gets a first-degree burn, they feel a lot of pain. This is because the damage only occurred on the surface.
A second-degree burn goes a little deeper and does more damage. They tell the nerves to send a louder signal to the brain.
However, people with third-degree burns often don’t experience any pain. This is because the burn damage went so deep, the nerves in the area were no longer able to send a message to the brain. Therefore no pain.
In other cases, the nerves can send TOO MUCH signal.
They tell the brain that there’s a big problem when there’s only a small problem.
Therefore, nerve pain can be very severe and often lasts for many months. It causes periodic shooting pain often described as bolts of lightning or electricity.
Examples of Nerve Pain Include:
- Trigeminal neuralgia
- Shingles pain
- Diabetic neuralgia
- Spinal cord injury
- Stroke pain
Nerve pain is one of the most common causes of chronic lower back pain.
Psychosomatic Pain
Has anybody ever told you that your pain is all in your head?
Psychosomatic pain is a type of pain that originates in the mind, rather than the body.
This type of pain is especially hard to treat with conventional medicine because although the feeling is real, there is no physical source to treat.
For this reason, most psychosomatic pain is chronic because of a “lack of effective treatment options”.
There are, however, a few excellent ways of treating psychosomatic pain if you know where to look.
(More on this in the next section)

Some examples of psychosomatic pain include:
- Chronic fatigue syndrome (CFS)
- Fibromyalgia
- Interstitial cystitis
- Body dysmorphic disorder.
- Stroke pain
Conventional Treatments For Pain
Humans have experienced pain for a long time.
Evidence suggests that we’ve been using the opium poppy for pain-relief as early as 3400 BCE.
This plant is the source of a special group of alkaloids with powerful pain management abilities.
In fact, we still use the active constituents of the opium poppy in modern medicine. It’s the source of things like codeine, fentanyl, and morphine.
5 Classes of Pain Medications Used in Hospitals
Opiates
Opiates are potent inhibitors of pain that stop the signal before they ever reach the brain by manually blocking the nerves in the spinal cord.
This class of drugs is used for all kinds of pain, including inflammatory, psychosomatic, and nerve pain.
Opiates are especially useful for nerve pain because it works by physically blocking nerve transmission itself, rather than another underlying factor.
Corticosteroids
The corticosteroid class of drugs are essentially “pain-relieving anti-inflammatories”. When inflammation goes down, pain follows.
Corticosteroids mimic some of our hormonal anti-inflammatory compounds to shut off inflammation.
They’re used for muscle pain, arthritis, as well as autoimmune conditions and allergies.
Benzodiazepines
This class of drugs are mainly used for treating anxiety, but also deliver some potent muscle relaxant activity.
They’re used to relieve pain associated with the muscles and joints such as arthritis, slipped discs, sports injuries, and spinal cord injuries.
Doctors also prescribe then alongside anxiety and with psychosomatic pain that also involves depression.
Antidepressants
Antidepressants are often used for treating psychosomatic pain due to a lack of other available treatment options. Studies have shown that the more depressed someone with psychosomatic pain feels, the more pain they ultimately experience.
Antidepressants are often used alongside fibromyalgia, chronic fatigue syndrome, Crohn’s disease, and interstitial cystitis.
NSAIDs
NSAID stands for “non-steroidal anti-inflammatory drugs”. This is what Aspirin and similar pain medications are classified as. They’re sold over the counter for mild pain and work by stopping inflammation.
NSAIDs are used for arthritis, back pain, and headaches.
The Problems with Conventional Pain Management

Although there are a lot of pain management options available in hospitals, they’re far from perfect.
Here are the most common problems with conventional pain management options:
They’re Often Addictive
Many of the best pain-relieving medications used in hospitals today are also highly addictive.
This is especially the case with opiates, benzodiazepines, and antidepressants.
All of these drugs work by acting on a specific receptor on a cell. It’s just like hitting a button.
If you hit the button too many times, the body adjusts by making it harder to press. This means that you’ll need to take more of the drug to produce the same effect.
If you stop taking the drug, the button is now too sticky to push it on your own. We push and push, but can’t activate it. This always leads to serious problems.

We call this withdrawal.
Many of the best pharmaceutical drugs will result in tolerance and withdrawal if taken for a long enough time.
Opiate withdrawal involves widespread pain and discomfort.
Benzodiazepine withdrawal involves severe panic attacks, heart palpitations, and insomnia.
Antidepressant withdrawal pushes us into a deeper depression than ever before.
As soon as the body starts to feel symptoms of withdrawal, it craves the drug that makes it go away.
This is what we call addiction.
They Don’t Address the Cause
Treating people for pain by disconnecting the body from the brain with opiates may help in the short term, but as soon as the drugs wear off the pain comes back just as strong as before.
In fact, sometimes the pain will come back EVEN WORSE than before as the drugs start to wear off.
They can Mess with Your Hormones
Corticosteroids are one of the most common forms of pain management in the hospital setting.
They mimic cortisone, which is an important hormone in the body.
Corticosteroids inhibit immune function, cause a loss of bone density, and make us gain weight. It can also lead to metabolic disorders like diabetes or high cholesterol over long periods of time.
Cushing’s syndrome is a condition brought on by long-term corticosteroid use. The condition is severe and often leads to long-term health problems.
30 Ways to Relieve Pain Naturally

There are plenty of excellent natural pain management options.
Every traditional medical system in the world has developed its own treatments for pain depending on the culture and the plants available to them.
The benefit of living in the modern era is that we can look back at all these different methods of pain management and figure out what’s going to work for your specific type of pain.
This list is compiled from the wealth of knowledge given to us by hundreds of years of trial and error and rigorous scientific testing.

This list includes herbs and techniques from:
- Traditional Chinese Medicine
- Ayurveda
- Nutritional Medicine
- Western Herbal Medicine
- Thomsonian Medicine
- Taoism
- Greek philosophy
Combining these old techniques with modern day research has allowed us to isolate the most effective natural pain relievers known to man.
So let’s begin!
Herbal Remedies
Herbs are like pharmaceuticals, but with some key differences.
Pharmaceuticals are a single isolated compound. They’re often synthesized in a lab. The compound has a specific effect on the body and usually targets a single receptor in the body.
Plants also contain chemicals, many of which have been isolated and turned into pharmaceutical medications.
But it gets so much better.
The raw plant itself often contains HUNDREDS of different chemicals.
The effects herb produces is the sum of its entire composition, all working together.
It’s a lot like an orchestra.
When a single instrument is playing, it sounds nice, no doubt. But when the entire orchestra plays together the experience becomes so much more. Herbs behave the exact same way.
Let’s dig a little deeper into how this works.
In many cases, herbs offer greater benefit because they don’t only push one button in the body to exert their effects. Instead, they use a concept called synergy.
This is where the numerous compounds in the plant work together to produce a stronger effect than any of them in isolation.
Just like an orchestra, each chemical has its own contribution:
- Some offer direct benefits (the brass)
- Some offer similar benefits but in a different way (the woodwinds)`
- Some eliminate side effects (the strings)
- Some improve absorption and elimination (the percussion)
This makes herbs a lot better at treating complex, hard to treat causes of pain. They tend to be slower than pharmaceuticals, but their effects last much longer.
Herbs also tend to have more corrective effects, treating the source of the problem rather than just the symptoms.
Herbs can be divided into a few different categories.
Topical Herbs
Topical herbs are useful for pain management involving the joints, muscles, and skin. They can exert their effects by numbing the site, reducing inflammation, or speeding recovery.
Somewhat ironically, herbs can also reduce pain and inflammation by CAUSING some mild inflammation. This last effect is referred to as rubefacient.
A rubefacient causes mild inflammation, which triggers the body’s natural anti-inflammatory response.
You can think of this through popular products like Tiger Balm. This product causes a warming sensation at first, which makes the pain and inflammation start to subside about an hour later.
They are extremely effective for joint and muscle pain and are one of the most commonly used topical herb treatments for pain and inflammation used by herbalists and professional athletes alike.
1. Cayenne Pepper
Cayenne pepper (Capsicum annuum) is best known for its use as a culinary spice, however, it’s also an extremely useful pain reduction herb.
The active ingredient, capsaicin, stimulates the heat receptors (vanilloid receptors), triggering the sensation of “heat”. When this happens, the body increases blood flow to the area. [21].
This makes cayenne a powerful rubefacient, causing mild inflammation and sensation of heat to the area it’s applied to. After about an hour, inflammation starts to go down, taking the pain along with it.
Cayenne pepper comes in the form of topical salves or rubs and is best used for treating:
- Muscle pain
- Sports injuries
- Lower back pain
- Joint pain
2. Mustard Seed
Mustard seed (Brassica nigra), like cayenne, is a rubefacient style pain remedy.
It contains as many as 50 different isothiocyanates which give mustard its characteristic flavor and aroma. They also provide the bulk of the pain-relieving benefits.
Mustard seed salve, oil or tinctures are used topically to increase blood flow to the joints. This helps it relieve arthritic and muscle pain.
3. Calendula
Calendula (Calendula officinalis) is a modest flower found growing throughout Europe and North America.
Its flowers petals are an excellent topical pain remedy.
Calendula is a potent anti-inflammatory [1], making it useful for treating pain caused by inflammation and irritation. It’s especially useful for pain involved with the skin.
It works by inhibiting an enzyme known as COX (cyclooxygenase), which is the same target for the common pharmaceutical anti-inflammatory and pain relief medication, Aspirin.
Calendula is useful as a topical pain reliever for conditions including:
- Arthritis
- Eczema
- Psoriasis
- Muscle pain
- Torn ligaments
- Scrapes and scratches
- Allergic reactions of the skin
It excels in treating any pain associated with the skin but also permeates deeper down to the muscles and ligaments over time.
4. Stinging Nettle
Stinging nettle (Urtica dioica) is one of the oldest herbal medicines in the world.
It’s used as a nutritional supplement for its high vitamin and mineral content and can be applied topically to reduce pain and irritation of the skin, joints, and muscles.
The leaves have thousands of tiny stinging hairs (hence its name). These hairs contain chemicals like histamine and serotonin, which cause an allergic reaction when it touches the skin.
People use stinging nettle by rubbing them on sore joints to relieve pain and inflammation of the affected area.
It may sound crazy,
But rubbing the irritating stinging nettle leaves on the skin actually cause counter-inflammation over time.
The effects of stinging nettle, when used in this way, are very powerful.
The effects last between 6 and 10 hours and tend to build over time, lasting longer with each treatment.
Stinging nettle is useful for treating:
- Rheumatoid arthritis
- Osteoarthritis
- Skin inflammation
- Lower back pain
- Muscle injur
- Torn ligaments
Analgesic Herbs (Pain Inhibitors)
Analgesic herbs reduce pain by directly affecting the nerves that transmit the pain signal to the brain.
They often work through the same receptors as pharmaceutical pain medications but tend to be more gentle and less addictive.
These herbs have more powerful pain-relieving qualities than other herb class.
They don’t work as quickly as their pharmaceutical counterparts but have longer-lasting effects and fewer side effects (if any).
5. California Poppy
California poppy (Eschscholzia californica) is a close relative of the opium poppy (Papaver somniferum). It contains similar chemicals, with comparable pain-relieving qualities.
Like pharmaceutical opiates, the alkaloids in California poppy work by stimulating the opioid receptors (though to a lesser degree).
It also works by increasing the potency of GABA in the nervous system, which is how pain-relieving benzodiazepine medications work.
When taking California poppy, you’re essentially using a natural combination of benzodiazepines and opiates, only with fewer side effects or potential for addiction.
California poppy is not addictive but can be very useful for treating general pain throughout the body. It’s great for treating chronic pain that other medications or herbs haven’t had any success in treating.
California poppy is useful for treating:
- Crohn’s disease/Ulcerative colitis
- Lower back pain
- Neck pain
- Torn ligaments
- Muscle injuries
- Cancer pain
- Migraine headaches
- Skin lacerations and bruises
- Fibromyalgia
- Chronic fatigue syndrome
- Interstitial cystitis
Many herbalists use it to relieve symptoms of pain while they address the cause with other herbs or supplements.
Don’t use California poppy if you’re pregnant or breastfeeding. Only adults can safely handle the analgesic alkaloids in the plant.
6. Kratom
Kratom (Mitragyna speciosa), like California poppy, works through the opioid receptors.
It’s effects are so strong, it’s actually used to treat opioid addiction by binding to the receptors, and reducing the withdrawal effects [25].
It binds to 2 out of the 3 types of opioid receptors in the spinal cord (mu- and delta-) cutting pain transmission off long before it ever reaches the brain. One of the active ingredients, 7-hydroxymitragynine, is even reported to be more potent than morphine. [24].
This makes kratom one of the greatest pain-relieving herbs of all time.
OK, I know what you’re thinking…
“If kratom binds to the opioid receptors more than morphine, it must be highly addictive”.
Although kratom can produce addictive qualities over time, it’s been shown on numerous occasions to have significantly less potential for addiction than other opioids [25], and is used to treat opioid addiction. Patients wean themselves off the drugs and onto kratom, which they can stop using much more easily.
7. Corydalis
Corydalis (Corydalis ambigua) is a popular herb brought to us by traditional Chinese medicine. It’s considered by many to be the second most effective pain reliever, only beaten by opium.
It’s active constituent, dehydrocorybulbine (DHCB), works by mildly stimulating the opioid receptors and inhibiting the dopamine receptors associated with the transmission of pain [2].
It’s especially useful for widespread chronic pain, such as:
- Fibromyalgia
- Chronic fatigue syndrome
- Rheumatoid arthritis
- Migraine headaches
- Nerve damage
- Cancer pain
Corydalis should NOT be used while pregnant or nursing as it is not safe for babies or small children.
8. Kava
Kava (Piper methysticum) is found naturally on many of the Islands scattered throughout the Pacific ocean.
Indigenous groups use kava for nerve pain, inflammation, rheumatoid arthritis, gout, and joint pain. It was also commonly consumed as a ceremonial drink to achieve higher levels of consciousness.
Modern uses of kava focus on its ability to relieve pain and calm the mind. It helps us alleviate stress.
Often times, the pain we experience is worsened by stress. When we relax, the pain goes away.
Kava is particularly useful for:
- Nerve pain
- Psychosomatic pain
- Headaches
- Urinary tract infection
- Pain associated with anxiety and depression
- Cancer pain
Kava is often used when other pain treatments haven’t worked. It’s one of the most reliable herbal pain relievers available.
9. CBD Oil (Hemp & Marijuana)
CBD is one of the active ingredients in marijuana & hemp plants (Cannabis indica/sativa).
It’s non-psychoactive meaning it won’t make you high.
CBD produces most of the medicinal benefits of the plant, including the pain relieving, antiepileptic, anti-anxiety, relieving arthritis joint pain, and anti-insomnia effects attributed to marijuana and hemp.
There are two main types of CBD oil available that you need to know about:
A) CBD Isolates
This is a pure CBD extract. All other cannabinoids, terpenes, and other phytochemicals are removed. This allows a higher dose of CBD to be taken and is most useful for treating epilepsy.
B) Full Spectrum Hemp Oil
Full spectrum hemp oil contains all phytochemicals contained in the hemp plant, including small amounts of the psychoactive THC (>0.03%).
There usually isn’t enough THC to produce any psychoactive effects.
This type of CBD oil is preferred in online and local shops for its pain-relieving benefits because it also provides other chemicals that work together to relieve pain and inflammation in the body. Phytochemicals like terpenes, minerals, flavonoids, and other cannabinoids all help to reduce pain and inflammation naturally and effectively.
CBD oils are good for all types of pain including nerve, inflammatory, and psychosomatic pain.
It works through the vanilloid receptors, endorphin/enkephalins, and through direct anti-inflammatory benefits [4].
Also, CBD-infused gummies are another way of consuming if you do not like the hempy taste of the oils.
CBD is useful for treating:
- Cancer pain
- Neuralgia
- Arthritis
- Muscle injuries or tension
- Headaches
- Multiple sclerosis
- Epilepsy
- Crohn’s disease
10. St John’s Wort
St John’s Wort (Hypericum perforatum) was one of the most important of the early European herbal medicines.
It was used as a treatment for depression and anxiety.
Modern research on the plant has backed up these traditional benefits and highlighted some new uses for it.
St John’s Wort was found to have the same mechanism of action as many of our common antidepressant medications (SSRIs).
This makes it especially useful for psychosomatic pain associated with psychological disorders and chronic stress, anxiety, or depression.
Its active ingredient, hypericin, was shown to work through the opioid receptors, but not directly.
Instead, it works through a system that regulates the opioid receptors called protein kinase C Gamma [5].
This allows St John’s Wort to produce significant pain relieving qualities without the negative side effects of addiction, tolerance, over-sedation, and gastrointestinal dysfunction common with conventional opiates.
St John’s Wort is useful for treating:
- Fibromyalgia
- Interstitial cystitis
- Chronic fatigue syndrome
- Tension headaches
- Pain with insomnia
- Depression
- Anxiety
- Viral infection
Anti-Inflammatory Herbs
Inflammation and pain almost always go hand in hand. This is why many of the best pain relieving herbs are actually inflammatories when you look at them closely.
There are a lot of anti-inflammatory herbs available. We’ll show you the ones that stand out above the rest for their ability to relieve pain.
Keep reading to find out.
11. Ginger
Ginger (Zingiber officinale) is one of the most well-rounded herbs available to us. It’s a potent anti-inflammatory pain reliever and is readily accessible at most local supermarkets.
Ginger root has many medicinal uses, all working together to reduce pain and inflammation.
Ginger’s effects include:
- Relieves gas and bloating (reduces stomach and digestive pain)
- Soothes upset stomach (lowers stomach pain)
- Reduces muscle tension (stops muscle pain)
- Stimulates blood flow (speeds muscle and joint repair)
- Lowers platelet aggregation (lowers arterial inflammation)
- Stimulates digestion (improves healing times and soothes upset stomach)
- Lowers inflammation (COX inhibitor similar to Aspirin)
- Kills invading bacteria (treats pain associated with infection)
All you need to do to use this herb for pain relief is to make a strong tea with the roots by boiling it in water for 15 or 20 minutes.
It’s especially useful for:
- Menstrual pain
- Arthritis
- Muscle aches and pains
- Nausea/vomiting
- Colic pain
- Stomach ulcers
- Muscle pains (topically)
- Digestive pain (like Crohn’s disease, diverticulitis, or ulcerative colitis)
12. White Willow Bark
White willow (Salix alba) is the original source for Aspirin. It’s often referred to as “nature’s Aspirin”.
The bark and leaves of the plant are high in a compound called salicylic acid. A scientific researcher in the late 1800’s isolated the compound, and was able to modify it slightly to produce Aspirin (Acetylsalicylic acid).
White willow is an excellent all around pain-reliever. It stops the formation of pro-inflammatory compounds by inhibiting the famous COX enzyme.
It’s useful for all kinds of pain, but is especially useful for treating:
- Joint pain
- Lower back pain
- Muscle damage
- Migraine headaches
- Menstrual pain
- Torn ligaments
- Insect bites (topically)
White willow should be avoided by anybody under the age of 6 due to a rare, but serious condition called Reye’s syndrome that can happen in children taking Aspirin or salicylic acid.
13. Turmeric
Turmeric (Curcuma longa) is one of the most well-studied plants on earth. It’s popular as both a food and medicine, with traditional use dating back over 4500 years.
The bright orange roots are high in antioxidants and anti-inflammatory compounds.
It inhibits something called phospholipase (A & D) which are important in the process of inflammation.
As a relative of ginger, it also improves blood flow to the site of injury and inhibits the COX enzyme [6-8].
Turmeric can be eaten as a food, taken in capsules or used as a liquid extract.
In order to get the pain-relieving benefits of turmeric, it needs to be taken high doses. Your turmeric lattes are great but not going to provide enough turmeric to give you any real benefits in terms of pain relief.
The best way to take turmeric is in capsules. We often double the dose listed on the bottle when targeting pain.
Turmeric is very safe and is traditionally eaten in very large amounts as food. You can also get turmeric tincture online.
Turmeric is especially useful for treating:
- Digestive system pain (Crohn’s disease and Ulcerative colitis)
- Arthritis
- Gout
- Asthma
- Eczema
- Psoriasis
- Throat infection
- Cancer pain
14. Devil’s Claw Root
Devil’s Claw (Harpagophytum procumbens) is famous in its native South Africa as a natural pain reliever and anti-inflammatory herb.
The long, fibrous roots resemble claws (hence the name).
The plant contains a group of chemicals known collectively as harpagosides. They’ve been shown to provide the bulk of the therapeutic benefits associated with devil’s claw.
A large, systematic review involving over 380 patients, concluded that there is “strong evidence” that devil’s claw is an effective treatment for non-specific lower back pain [21]. This study used devil’s claw at a dose containing 50 mg harpagosides (equivalent to about 4g per day of the raw herb).
Devil’s claw is especially useful for treating:
- Lower back pain
- Osteoarthritis
- Rheumatoid arthritis
- Tendinitis
- Athletic joint injuries
15. Frankincense
Frankincense (Boswellia serrata) is our favorite herb for arthritic pain.
Here’s why…
Frankincense is a potent anti-inflammatory and works to improve blood flow to the damaged cartilage that makes up arthritic joints.
It works by inhibiting an enzyme similar to COXcalled 5-LOX [9].
This enzyme, like COX, is used to build inflammatory compounds. 5-LOX particularly important, however, when it comes to the low-grade inflammation driving osteoarthritis.
By inhibiting 5-LOX, especially in combination with other anti-inflammatories like turmeric or ginger, frankincense can stop the inflammation driving osteoarthritis. It can reduce joint pain substantially over time and addresses many of the underlying causes of the condition.
It takes a few weeks for frankincense to produce benefits, so many people choose to keep taking their normal pain meds for the first couple of weeks until they start to see improvements.
Frankincense is useful for treating:
- Osteoarthritis
- Crohn’s disease
- Cancer pain
- Systemic lupus erythematosus (SLE)
- Headaches
16. Borage Seed Oil
Borage (Borago officinalis) seed oil owes its pain-relieving benefits to a compound called GLA.
GLA (gamma-linoleic-acid) is an omega 6 fatty acid with hormone-like anti-inflammatory activity.
A recent study involving 203 patients with spinal pain showed a significant reduction in symptoms with 420 mg of GLA in the treatment group compared to placebo [23].
Borage seed oil and its active ingredient, GLA, work by lowering inflammation, and boosting the process of repairing damaged nerve fibers.
Borage seed oil is useful for treating conditions such as:
- Chronic back pain
- Nerve damage
- Rheumatoid arthritis
- Osteoarthritis
- Eczema and irritated skin
- Premenstrual pain
- Sore throat and lungs
Adrenal Tonic Herbs
There is a lot more going on when you feel pain than you might think.
We’re about to discuss one of the most overlooked methods of pain management.
Our adrenals.
Almost nobody is talking about this important method of pain management despite there being a ton of evidence to support it.
How does this work?
The adrenal glands control our fight or flight response and are important for regulating both inflammation and neurotransmitter function.
The adrenals are crucial for helping us adapt to our environment, and resist many different kinds of stress, including the stress brought on by pain.
With the level of stress people are often under in the modern world, It’s becoming a lot more common to see a condition called “adrenal exhaustion”.
When this happens, our ability to resist stress starts to fail.
With our adrenals no longer working properly, our perception of pain skyrockets and can become unbearable.
This is often what is happening in a lot of chronic and mysterious causes of pain like fibromyalgia and chronic fatigue syndrome.
17. Ashwagandha
Ashwagandha (Withania somnifera) is perhaps the best adrenal tonic herb of all time.
It’s extremely gentle, and is often used on pregnant mothers and small children. It doesn’t “stimulate” the adrenals– it builds them up, making them stronger and more resilient.
Studies have shown it can lower the amount of the stress hormone, corticosterone, in our blood. It can regulate our immune function. This works to lower inflammation and help us cope with pain more easily. [10].
Ashwagandha is especially useful for treating pain associated with:
- Headaches
- Chronic fatigue syndrome
- Fibromyalgia
- Multiple sclerosis
- Severe anxiety
- Hypothyroidism
- Infection
- Muscle injuries
- Drug abuse
- Pregnancy
18. Rehmannia
Rehmannia (Rehmannia glutinosa) is an extremely valuable herb for the adrenals. It’s perfect for the modern era of chronically stressed, burnt out people.
It contains a series of natural corticosteroid-like compounds that work to enhance the way our brains respond to stress. It tones the adrenal glands and makes us more resilient overall.
This is one of the few herbs we take every day, especially when we’re feeling particularly stressed out.
It also provides useful anti-inflammatory effects through a similar method to pharmaceutical corticosteroids, only without the negative side effects.
Rehmannia is useful for treating pain associated with:
- Chronic fatigue syndrome
- Fibromyalgia
- Depression/anxiety
- Cancer
- Constipation
- Kidney disease
- HIV
- Multiple sclerosis
- Chronic stress
- Arthritis
- Allergies
- Eczema & psoriasis
Rehmannia is often used alongside other pain relievers to help the body respond and adapt to stress more easily. It helps other herbs work their magic towards reducing pain and inflammation.
Nervines
Nervines are a class of herbs specific to the nervous system.
There are a million different ways nervines can exert their benefits, but all will offer some form of improvement to nerve health or function.
This class of herbs is especially important when managing nerve pain, but can also be useful for other forms of pain, especially since it’s the nerves job to transmit pain signals to the brain.
19. Lion’s Mane
If you were to ask a herbalist what the best nervine for nerve damage is, they’d likely tell you it’s lion’s mane mushroom (Hericium erinaceus).
This incredible fungus grows off the sides of pine and spruce trees and looks like a big ball of white fur. Hence the common name, lion’s mane.
What makes this fungus amazing is its ability to stimulate something called nerve growth factor… NGF for short.
This compound stimulates the growth and repair of neurons inside the brain, down the spinal cord, and out into the body.
Animal studies have shown that lion’s mane can speed up the repair process of damaged nerve fibers significantly [25].This helps treat the cause of nerve-related pain, and can gradually reduce tough to treat chronic nerve pain over time.
Lion’s mane is useful for treating pain associated with:
- Multiple sclerosis
- Parkinson’s disease
- Neuralgia
- Stroke
- Concussion
- Brain damage
- Spinal cord injury
- Shingles virus
- Herpes virus
- HIV
- Cancer
- Sciatica pain
20. American Skullcap
American skullcap (Scutellaria lateriflora) is considered the “king of the nervines”.
Susan Weed, a famous American herbalist, suggests that “Skullcap tincture relieves almost any pain, especially when the nerves are involved.
Try skullcap when bothered by pain involved with conditions such as:
- Sciatica pain
- Neuralgia
- Toothaches
- Eye Twitches
- Ringing in the ears
- Spinal cord injuries
- Lower back pain
- Depression/anxiety
- Chronic fatigue syndrome
- Fibromyalgia
You can get skullcap in the form of a tea or a tincture, and both are great, however, the best option is a tincture made from the fresh plant.
This is because many of the pain-relieving and nervine qualities of the plant are thanks to its volatile oil content.
Although still present in dried herbs, much of the volatile components evaporate as they dry up.
Nutritional Supplements

We can’t talk about pain management in depth if we don’t talk about nutrition.
This is extremely important to keep in mind whenever managing pain because everything our body does requires ingredients obtained from the diet.
If we’re not eating the right foods, we’re going to start developing problems.
As you might know already, whenever there’s a problem in the body, it sends a signal to the brain in the form of pain.
This is why proper nutrition and supplementation can go a long way in preventing and treating pain at its source.
21. Magnesium
Magnesium is very important. It’s used in well over 300 different enzyme reactions in the body. These enzymes regulate everything from neurotransmitter production to muscle contraction.
When we don’t have enough magnesium, we start to develop headaches, muscle tension, and insomnia. It can even lead to more serious conditions like fibromyalgia [11].
Magnesium inhibits something called substance P, which is used to transmit pain signals to the brain. This is one of the ways opiates treat pain. The activated opiate receptors inhibit substance P, thus preventing the pain signal from reaching the brain [12].
You can get magnesium through supplementation, or by eating more foods that contain magnesium.
Foods High In Magnesium:
- Walnuts
- Almonds
- Dark chocolate
- Avocado
When supplementing magnesium, we prefer to use magnesium glycinate due to its high bioavailability, reasonable price, and high weight of elemental magnesium (pure magnesium) per gram.
Magnesium is useful for treating pain related to:
- Muscle injury/Tension
- Migraine or tension headaches
- Anxiety/Stress
- Cancer
- Neuralgia
- Shingles virus
- Herpes virus
22. Fish Oil
Fish oil is high in omega 3 essential fatty acids.
There are actually 2 types of omega fatty acids; Omega 3 from fish and seeds, and omega 6 from vegetable oils and eggs.
The optimal ratio of the omega 6 to omega 3 is 1:1.
The modern diet is much higher in omega 6 than it is in omega 3, somewhere around 15:1 on average [13].
The problem with this is that omega 6 is used to promote inflammation, while omega 3 is used to stop it. This happens with the help of the COX enzyme talked about previously.
With so little omega 3 available in the modern diet, our body enters a painful inflammatory state but has a hard time getting back out of it when it’s no longer needed.
Supplemental fish oil has been shown to reduce pain associated with arthritis [14], and inflammation from autoimmune diseases [15].
Studies have shown that fish oil is able to reduce arthritic back & joint pain as effectively as Aspirin while being significantly safer [16, 17].
Fish oil is useful for treating pain associated with:
- Neck/Back pain
- Arthritis
- Multiple sclerosis
- Cancer
- Heart disease
- Muscle or ligament injury
- Neuralgia
There’s something very important to keep in mind when buying fish oils though:
Make sure you only order high-quality products that have been properly stored in the fridge. Cheap fish oils are notorious for spoilage, which won’t have any effect on pain.
23. Bromelain
Bromelain is naturally produced in the bromeliad family of plants. The most famous member of this family is the pineapple (Ananas comosus).
It’s an enzyme that helps us break down proteins in our digestive tract.
But that’s not all it’s good for.
Bromelain has also recently been shown to have potent pain-relieving and anti-inflammatory properties [22].
Its effects are similar to Aspirin, only MUCH better. Here’s how it works:
Aspirin blocks the COX enzyme, which is responsible for producing both pro-inflammatory messengers, and anti-inflammatory messengers. Bromelain works further down the pathway and ONLY blocks the pro-inflammatory messengers.
This shifts the balance from promoting inflammation to preventing or stopping inflammation.
As mentioned in other sections, when inflammation goes down, so does the pain.
Bromelain has many benefits, the main ones include:
- Reduces inflammation
- Relieves inflammatory pain
- Prevents cancer cell growth
- Improves protein digestion
- Relieves stomach pain
- Supports the cardiovascular system
24. Alpha Lipoic Acid
Alpha lipoic acid is an antioxidant with powerful benefits towards treating nerve pain including damaged spinal discs.
As many as 80% of chronic back pain is associated with disc dysfunctions [19].
This causes damage to the nerve roots located in the spinal cord, causing severe, often debilitating pain the lower back.
Alpha lipoic acid is produced naturally in the body but is often given in high doses to relieve pain originating in the nerves.
Doses of just 300 mg per day of alpha lipoic acid (ALA) has been shown to reduce neuralgic back pain by raising the pain threshold in the nerves [18].
It also reduces tingling sensations in the hands, feet, and legs.
ALA is useful for treating pain associated with:
- Nerve damage
- Spinal disc injuries
- Neuralgia
- Lower and upper back pain
- Neck pain
25. L-Glucosamine & Chondroitin Sulphate
Glucosamine and chondroitin sulfate are the two most popular nutritional supplements for arthritic joint pain.
As arthritis develops, the cartilage in the joints breaks down.
This cartilage is important for lowering friction between the bones connecting at a joint and prevents them from rubbing directly against each other.
As it breaks down, it starts to cause pain and inflammation, resulting in further degeneration of the cartilage. It’s a problem that ends up feeding itself, making the problem exponentially worse over time.
Glucosamine and chondroitin sulfate form the major building blocks for cartilage in the joints. They help regenerate lost cartilage, offering direct pain-reducing effects in the joints with long term treatment.
These supplements address the source of arthritic pain to provide long-lasting benefits.
Chondroitin sulfate and L-Glucosamine are used to treat pain associated with:
- Osteoarthritis
- Rheumatoid arthritis
- Hip replacement surgery
- Lower back pain
- Neck pain
- Joint injuries
Sometimes these 2 supplements are sold together, other times you need to buy them individually. We recommend taking both supplements at the same time for best results.
Lifestyle Changes (Physical and Psychological)
Physical Therapies
A major part of the healing process relies on body movement.
The muscles and joints rely on movement to help wash out harmful metabolic byproducts like lactic acid and free radicals.
Inflammation also relies on movement to help with lymphatic drainage during recovery.
For this reason, physical therapies are an extremely important factor to consider adding to your pain management regimen.
26. Yoga
Yoga helps with pain management in several ways:
A) It allows for a gentle movement of the body to help increase blood flow to damaged and inflamed areas of the body, thus reducing pain and inflammation
B) It promotes deep breathing, which calms the body and reduces stress, thereby improving our ability to resist pain.
C) It helps change our perception of pain through body awareness and mental discipline.
For best results, try a gentle yoga practice like yin restorative yoga. If you overexert yourself while in pain, you can cause more harm to your body than good.
Slow, gentle yoga is best for managing pain and has the most relaxing benefits.
27. Massage Therapy
Massage therapy forces blood and lymph to move around in the body’s tissues, clearing out toxic metabolites and bring oxygen and nutrients into the area.
Therapeutic massages are one of the best methods of reducing muscle pain, and can even relieve some inflammation.
It’s important to find a professional massage therapist, however, rather than a friend or significant other. Especially with conditions like chronic fatigue syndrome of fibromyalgia.
A bad massage can actually make your problems with pain worse.
28. Acupuncture
Acupuncture is well-known for its pain-relieving benefits.
It works by activating endorphins in the body which change the body’s response to pain. It also increases blood flow and helps damaged, painful nerves repair themselves more quickly.
One study showed a 36% reduction in overall pain scores after 6 weeks of treatment with acupuncture [20].
Acupuncture is especially useful for:
- Chronic nerve pain
- Almonds
- Low back pain
- Cancer pain
Philosophy Changes
A lot of the experience of pain comes down to how our brains convert signals sent from elsewhere in the body.
The pain travels up the nerve fibers to our spinal cord, which injects them deep into the brain. Once in the brain, it’s translated and the sensation of pain then becomes evident.
Herbs and nutrition help with the source of pain, and the transmission of pain through the nerve fibers, but philosophical changes can address how the signal is actually converted in the brain.
This is extremely powerful, and should not be overlooked as a method of pain management.
It’s allowed Buddhist monks to endure significant pain on several occasions;
A Buddhist monk named Thích Quảng Đức in Vietnam burned himself alive as a protest to the way his government was treating Buddhist’s at the time.
His control over his mind was so strong, he didn’t make a sound or move a muscle as he sat in the street, burning alive.
This was also done in Tibet by other Buddhists after China’s occupation of Tibet.
29. Meditation
A few thousand years ago, the Buddha allegedly sat underneath the Bodhi tree, deep in meditation.
His only goal was to escape the pain and suffering of life and death. After several hours, he attained nirvana, the highest level of consciousness a human can achieve.
Meditation is a practice of mindfulness and self-awareness.
It teaches you to look deep within your thoughts and emotions to understand where they come from, and how to control them.
With meditation, we can rewire our own brains, including how we perceive pain. With practice, it can turn down the volume on how we perceive pain without the need for medications.
Of course, meditation is a practice and not something we’re naturally experts in. Just like other practices like painting, carpentry, or exercise, we need to do it often to improve the skill.
The more often you meditate, the more profound its benefits become.
30. Stoicism
Nobody likes to feel pain, there’s no doubt about it… right?
One philosophy might disagree.
Stoicism seeks to “embrace the suck” if you will.
They use pain and discomfort as a way to better themselves as people. They don’t create pain for themselves, but when it happens out of their control they use it as a source of strength rather than a source of weakness.
Seneca, one of the greatest stoic thinkers in history says it best— “misfortune is virtue’s opportunity”.
What he’s implying here is that when something bad happens, we can either let it drag us down… OR… we can use it to practice our patience & resilience.
Stoicism helps us become better at avoiding problems in the future and becoming more virtuous humans by enduring pain and struggle.
Conclusion
Millions of people around the world suffer from pain every day.
Often times they’re lead to believe that there is no cure and that they need to stay on pharmaceutical pain medications for the rest of their lives.
This couldn’t be further from the truth.
There are many effective ways of relieving pain naturally.
Every medical system in history has developed their own methods of relieving pain. Herbs, nutritional supplements, physical therapies, and philosophies have all been developed specifically for treating the discomfort of pain.
The key to doing it successfully is to be patient, and persistent.
Natural approaches to pain management tend to be slower, but their effects last much longer.
References
- Dall’Acqua, S., Catanzaro, D., Cocetta, V., Igl, N., Ragazzi, E., Giron, M. C., … & Montopoli, M. (2016). Protective effects of ψ taraxasterol 3-O-myristate and arnidiol 3-O-myristate isolated from Calendula officinalis on epithelial intestinal barrier. Fitoterapia, 109, 230-235.
- Zhang, Y., Wang, C., Wang, L., Parks, G. S., Zhang, X., Guo, Z., … & Borrelli, E. (2014). A novel analgesic isolated from a traditional Chinese medicine. Current Biology, 24(2), 117-123.
- Johnson, J. R., Burnell-Nugent, M., Lossignol, D., Ganae-Motan, E. D., Potts, R., & Fallon, M. T. (2010). Multicenter, double-blind, randomized, placebo-controlled, parallel-group study of the efficacy, safety, and tolerability of THC: CBD extract and THC extract in patients with intractable cancer-related pain. Journal of pain and symptom management, 39(2), 167-179.
- Russo, E. B. (2008). Cannabinoids in the management of difficult to treat pain. Therapeutics and clinical risk management, 4(1), 245.
- Galeotti, N., Vivoli, E., Bilia, A. R., Vincieri, F. F., & Ghelardini, C. (2010). St. John’s Wort reduces neuropathic pain through a hypericin-mediated inhibition of the protein kinase C γ and ɛ activity. Biochemical pharmacology, 79(9), 1327-1336.
- Goel, A., Boland, C. R., & Chauhan, D. P. (2001). Specific inhibition of cyclooxygenase-2 (COX-2) expression by dietary curcumin in HT-29 human colon cancer cells. Cancer letters, 172(2), 111-118.
- Yamamoto, H., Hanada, K., Kawasaki, K., & Nishijima, M. (1997). Inhibitory effect of curcumin on mammalian phospholipase D activity. FEBS letters, 417(2), 196-198.
- Rao, C. V., Rivenson, A., Simi, B., & Reddy, B. S. (1995). Chemoprevention of colon carcinogenesis by dietary curcumin, a naturally occurring plant phenolic compound. Cancer research, 55(2), 259-266.
- Gupta, I., Parihar, A., Malhotra, P., Singh, G. B., Lüdtke, R., Safayhi, H., & Ammon, H. P. (1997). Effects of Boswellia serrata gum resin in patients with ulcerative colitis. European journal of medical research, 2(1), 37-43.
- Bhattacharya, S. K., & Muruganandam, A. V. (2003). Adaptogenic activity of Withania somnifera: an experimental study using a rat model of chronic stress. Pharmacology Biochemistry and Behavior, 75(3), 547-555.
- Romano, T. J., & Stiller, J. W. (1994). Magnesium deficiency in fibromyalgia syndrome. Journal of nutritional medicine, 4(2), 165-167.
- Aicher, S. A., Punnoose, A., & Goldberg, A. (2000). μ-Opioid receptors often colocalize with the substance P receptor (NK1) in the trigeminal dorsal horn. Journal of Neuroscience, 20(11), 4345-4354.
- Simopoulos, A. P. (2002). The importance of the ratio of omega-6/omega-3 essential fatty acids. Biomedicine & pharmacotherapy, 56(8), 365-379.
- Kremer, J. M., Lawrence, D. A., Jubiz, W., Digiacomo, R., Rynes, R., Bartholomew, L. E., & Sherman, M. (1990). Dietary fish oil and olive oil supplementation in patients with rheumatoid arthritis clinical and immunologic effects. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology, 33(6), 810-820.
- Simopoulos, A. P. (2002). Omega-3 fatty acids in inflammation and autoimmune diseases. Journal of the American College of nutrition, 21(6), 495-505.
- Maroon, J. C., & Bost, J. W. (2006). ω-3 Fatty acids (fish oil) as an anti-inflammatory: an alternative to nonsteroidal anti-inflammatory drugs for discogenic pain. Surgical neurology, 65(4), 326-331.
- Goldberg, R. J., & Katz, J. (2007). A meta-analysis of the analgesic effects of omega-3 polyunsaturated fatty acid supplementation for inflammatory joint pain. Pain, 129(1-2), 210-223.
- Ranieri, M., Sciuscio, M., Cortese, A. M., Santamato, A., Di Teo, L., Ianieri, G., … & Megna, M. (2009). The Use and Alpha-Lipoic Acid (ALA), Gamma Linolenic Acid (GLA) and Rehabilitation in the Treatment of Back Pain: Effect on Health-Related Quality of Life. International journal of immunopathology and pharmacology, 22(3_suppl), 45-50.
- Yin, W., & Bogduk, N. (2007). The nature of neck pain in a private pain clinic in the United States. Pain Medicine, 9(2), 196-203.
- Molassiotis, A., Sylt, P., & Diggins, H. (2007). The management of cancer-related fatigue after chemotherapy with acupuncture and acupressure: a randomised controlled trial. Complementary therapies in medicine, 15(4), 228-237.
- Gagnier, J. J., Chrubasik, S., & Manheimer, E. (2004). Harpgophytum procumbens for osteoarthritis and low back pain: a systematic review. BMC complementary and alternative medicine, 4(1), 13.
- Taussig, S. J., & Batkin, S. (1988). Bromelain, the enzyme complex of pineapple (Ananas comosus) and its clinical application. An update. Journal of ethnopharmacology, 22(2), 191-203.
- Ranieri, M., Sciuscio, M., Cortese, A. M., Santamato, A., Di Teo, L., Ianieri, G., … & Megna, M. (2009). The Use and Alpha-Lipoic Acid (ALA), Gamma Linolenic Acid (GLA) and Rehabilitation in the Treatment of Back Pain: Effect on Health-Related Quality of Life. International journal of immunopathology and pharmacology, 22(3_suppl), 45-50.
- Babu, K. M., McCurdy, C. R., & Boyer, E. W. (2008). Opioid receptors and legal highs: Salvia divinorum and Kratom. Clinical Toxicology, 46(2), 146-152.
- Boyer, E. W., Babu, K. M., Adkins, J. E., McCurdy, C. R., & Halpern, J. H. (2008). Self‐treatment of opioid withdrawal using kratom (Mitragynia speciosa korth). Addiction, 103(6), 1048-1050.
- Wong, K. H., Naidu, M., David, R. P., Abdulla, M. A., & Kuppusamy, U. R. (2009). Functional recovery enhancement following injury to rodent peroneal nerve by Lion’s Mane mushroom, Hericium erinaceus (Bull.: Fr.) Pers.(Aphyllophoromycetideae). International Journal of Medicinal Mushrooms, 11(3).










